Welcome to the 2024 Interprofessional Cross-Campus Collaborative Case
This case collaborative provides you with the opportunity to work in an interprofessional team of students from different health and social care professions.
Working together, your team will identify the needs of Cody James and his family and will build an interprofessional team to meet their needs.
Your team is tasked with ensuring the delivery of holistic, whole person, interprofessional team-based care to meet the physical, emotional and social needs of Cody James and his family.
Case timelines by location
Case timeline - Missouri
Registration opens Friday, August 30, 2024
Orientation
● Wednesday, Oct. 09, 7:30 - 8:30 p.m. Live via Zoom
Workshop 1 and 2
● Wednesday, Oct. 16, 7:00 - 9:00 p.m. Live via Zoom and recorded.
Workshop 3
● Wednesday, Oct. 23, 7:00 - 8:00 p.m. Live via Zoom and recorded.
Practice Sessions
● October 28th through November 8, 2024 Live via Zoom
Final Presentations
● Week of Nov. 11 - Nov. 15, Live via Zoom
Reflection and Recognition Reception
● Wednesday, Dec. 4, 7:30 - 8:30 p.m., Live via Zoom
Case timeline - Arizona
Registration opens Friday, August 30, 2024
Orientation
● Wednesday, Oct. 09, 5:30 - 6:30 p.m. Live via Zoom
Workshop 1 and 2
● Wednesday, Oct. 16, 5:00 - 7:00 p.m. Live via Zoom and recorded.
Workshop 3
● Wednesday, Oct. 23, 5:00 - 6:00 p.m. Live via Zoom and recorded.
Practice Sessions
● October 28th through November 8, 2024 Live via Zoom
Final Presentations
● Week of Nov. 11 - Nov. 15, Live via Zoom
Reflection and Recognition Reception
● Wednesday, Dec. 4, 6:30 - 7:30 p.m., Live via Zoom
Case timeline - California
Registration opens Friday, August 30, 2024
Orientation
● Wednesday, Oct. 09, 5:30 - 6:30 p.m. Live via Zoom
Workshop 1 and 2
● Wednesday, Oct. 16, 5:00 - 7:00 p.m. Live via Zoom and recorded.
Workshop 3
● Wednesday, Oct. 23, 5:00 - 6:00 p.m. Live via Zoom and recorded.
Practice Sessions
● October 28th through November 8, 2024 Live via Zoom
Final Presentations
● Week of Nov. 11 - Nov. 15, Live via Zoom
Reflection and Recognition Reception
● Wednesday, Dec. 4, 5:30 - 6:30 p.m., Live via Zoom

Your Team Task
Your team is about to take over the care of Cody James, who was seen in the Urgent Care. He presented with acute right wrist pain following a fall during a soccer game and was diagnosed with right proximal middle phalanx Salter-Harris II fracture, Grade 2 acromioclavicular sprain of right shoulder, fatigue, leukocytosis, thrombocytopenia, erythrocytopenia, bruising with minimal to no trauma, frequent nosebleeds, and frequent URIs. He was subsequently diagnosed with Acute Lymphocytic Leukemia.
You are provided with the following information to help you with your task.
- Audio and written narratives from patient Cody James, mother Kristi James, and Cody’s sister Kelly James.
- A description of Cody James’ hometown.
- Documentation from the health professions involved in Cody’s care during his hospital stay.
Your team is tasked with:
- Identifying the holistic needs of Cody James and his family.
- Building an interprofessional team with the skills to meet the needs of Cody James and his family
As you work together to build the team to care for Cody James and his family you must consider:
- The holistic needs of Cody James and his family.
- How you can place the interests of Cody and his family at the center of the interprofessional team.
- The composition of the interprofessional team, identifying the roles and responsibilities of those involved and how they relate to the identified needs for this family.
- Specific team strategies you will use to ensure the interprofessional team functions as an effective team.
- Specific communication strategies the team will use to ensure they practice effective interprofessional communication.
- How quality improvement and patient safety will be addressed by the team.
The core competencies for interprofessional collaboration
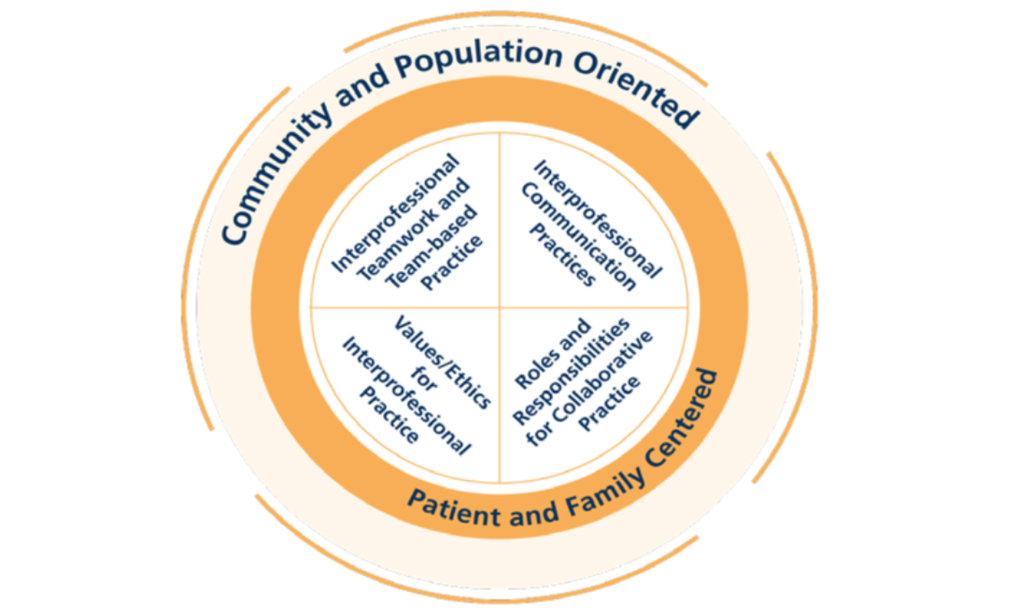
Use the 4 core competencies for interprofessional collaborative practice to guide you on the issues to consider:
- Work with individuals of other professions to maintain a climate of mutual respect and shared values. (Values/Ethics for Interprofessional Practice)
- Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. (Roles/Responsibilities)
- Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. (Interprofessional Communication)
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. (Teams and Teamwork)

Teams
Once you register for the collaborative event, you will be placed into a small interprofessional team and will be assigned a team facilitator. Names and contact information for your teammates and facilitator will be sent to you prior to orientation. By the end of the orientation event, your team should have developed a plan as to how you will communicate and function to complete the assigned tasks.
Interaction with Facilitators
A faculty team facilitator will be assigned to each team. The faculty team members who developed the case will serve as facilitators for your group and can help guide you through the task. So please feel free to ask for help in understanding the assigned task. Your facilitator is able to:
- Provide feedback/guidance to your team as you work through the case and prepare your presentation.
- Review your plan/presentation prior to your final team presentation.
- Provide feedback and comments during your practice session.
The Presentations
Your end product is an oral presentation, presented via Zoom, which demonstrates your reflection on the life story and care of Cody James and his family, and the professionals you would include in an interprofessional team to meet their needs.
You are also asked to provide a short reflective piece in your presentation on your own team's experience of collaboration in action, including what you have learned about the other professions' roles and responsibilities, team working, and communication issues.
Presentation Structure
Each team will have 20 minutes to present their work. A 5-minute, 3-minute and 1-minute warning will be given to the team. At the conclusion of 20 minutes, the timekeeper will announce time and your team must stop their presentation. No team will be permitted to exceed the allocated 20-minute time limit. If the team completes its presentation prior to the 20-minute time limit, the team should announce that they have completed their presentation. Presentations will be followed by a 10-minute question and answer period with a panel of judges.
Each team member must participate equally in both the oral presentation and the question and answer period immediately following the team presentation.
Teams are encouraged to invite friends and other students to attend their presentation. By the time of your scheduled rehearsal, please let your facilitator know the names and email addresses of any people you would like to invite. The audience may include other non-participating students, faculty, and interested health professionals. Audience members are requested not to ask questions or use the chat feature during the presentations.
Judges will complete a scoring sheet for each team presentation. An average score will be calculated for each team. Teams will be provided with their team score and feedback after the event.
Grading Rubric (download)
Cody James (The Case)

About Cody James (The Case)
Cody James is 11 years old and lives in Mesa, Arizona. He is a sixth grader at Bush Elementary School and plays soccer with the Mesa Youth Sports League. Cody was seen in the Urgent Care following a collision with an opponent on the soccer field. He presented with sharp pain in the wrist and digits of his right hand with swelling of the wrist and could not move the hand or wrist without severe pain. He was diagnosed with right proximal middle phalanx Salter-Harris II fracture, Grade 2 acromioclavicular sprain of right shoulder, fatigue, leukocytosis, thrombocytopenia, erythrocytopenia, bruising with minimal to no trauma, frequent nosebleeds, and frequent URIs.
Listen to Cody’s Urgent Care narrative (audio file)
Read Cody’s Urgent Care narrative (pdf)
Listen to Cody’s Follow Up narrative (audio file)
Read Cody’s Follow Up narrative (pdf)
Listen to Cody’s Mother’s narrative (audio file)
Read Cody’s Mother’s narrative (PDF)
Listen to Cody’s Sister’s narrative (audio file)
Read Cody’s Sister’s narrative (PDF)
Cody’s home town of Mesa, Arizona
General City Information: Mesa is located in Maricopa county in south-central Arizona. It is a southeastern suburb of Phoenix. With a population of more than 508,000 people, Mesa is the 36th largest city in the U.S. and second largest in the Phoenix metro area. It has seen significant population growth due to factors such as its warm climate, affordable housing and job market.The site was settled and founded in 1878 by Mormons who used ancient Hohokam canals for irrigation. Mesa Community College and the University of AZ’s Agricultural Experimental Station are located in Mesa. Salt River Pima-Maricopa Indian Community is across the river to the north.
School Information: Mesa has 15 public schools and Cody attends Bush Elementary in the Mesa Public Schools District. Bush has nearly 600 students enrolled in grades PK-6, with a student/teacher ratio of 14.34. There is a diverse enrollment in the school, though 65% are white, with 23% Hispanic, 4% black and a smattering of American Indian/Alaskan Native, Asian, and Native Hawaiian/Pacific Islander students. Bush has a Special Education Team that commits to creating and refining systems that support learning and social emotional competence at the classroom level. The team advocates that all students have an individualized learning experience that prepares them to meet their goals.
Medical & Psychiatric Healthcare in the region: Mesa has multiple urgent care centers with average costs variable, but ranging generally between $100 and $240.
One of the largest and most comprehensive hospital facilities in AZ is Banner Desert in Mesa, which treats the highest levels of acuity in the East Valley. Banner Health has comprehensive pediatric primary care and their pediatric psychiatry specialists treat depression and eating disorders (among a number of other emotional, behavioral and developmental disorders) in children and teens. Also part of the Banner Desert Medical Center, Banner Children’s Blood and Cancer Center serves children, adolescents and young adults who have blood problems (hematology) and cancer (oncology). They provide a team of expert board-certified physicians, advanced specialty certified practice nurses, social workers, a child life specialist, a nutritionist, and other health care professionals who work as a team with patients and families to help them heal and optimize their quality and length of life.
Additionally, the nearby Mayo Clinic Hospital in Phoenix was ranked as the #1 hospital in AZ by the U.S. News & World Report’s 2023 list of Best Regional Hospitals.
Phoenix Children’s Hospital of Phoenix also has Phoenix Children’s Specialty Care located in Mesa, Arizona, where pediatric patients can be seen by a number of different physician specialties, such as Center for Cancer & Blood Disorders, Neurology, Physical Medicine & Rehabilitation, and many others.
Sports in Mesa: Mesa offers a number of youth sports opportunities. Cody plays soccer with the Mesa Youth Sports league. Fee assistance of 50% discount is available with adequate documentation. In the past, the James family has never required this assistance, but with the current medical crisis, it may be necessary when Cody is able to return to soccer.
The Chicago Cubs have their spring training camp in Mesa and Cody and his family enjoy watching the Cubs practice at least once every spring.
Economics: Mesa’s cost of living is higher than the national average in some areas, including housing (17%), utilities (3%), and transportation (7%). However, healthcare in Mesa is 7% lower than the national average. In Mesa, it takes an hourly wage of $49.38 or an annual salary of $102,710 for a single adult to sustain comfortable living standards. For a household of four, it takes about $238,500.
Though Cody’s family’s income is significantly less than $238,000, they are fortunate to have inherited Cody’s father’s family home; thus, the only costs associated with their living expenses are taxes and utilities and general maintenance and repair of the older home (which can be significant at times), allowing them to maintain a middle class lifestyle when not challenged by emergency expenses.
Cody James’ Urgent Care Visit
Cody James was seen in an Urgent Care Center following a collision with an opponent on the soccer field. He presented with sharp pain in the wrist and digits of his right hand with swelling of the wrist and could not move the hand or wrist without severe pain. He was diagnosed with right proximal middle phalanx Salter-Harris II fracture, Grade 2 acromioclavicular sprain of right shoulder, fatigue, leukocytosis, thrombocytopenia, erythrocytopenia, bruising with minimal to no trauma, frequent nosebleeds, and frequent URIs.As part of Banner Desert Medical Center, Banner Children’s Blood and Cancer Center serves children, adolescents and young adults who have blood problems (hematology) and cancer (oncology). They provide a team of expert board-certified physicians, advanced specialty certified practice nurses, social workers, a child life specialist, a nutritionist, and other health care professionals who work as a team with patients and families to help them heal and optimize their quality and length of life.
Click here for more information on Banner Desert Medical Center.
Physician/PA Urgent Care Note
Cody James Urgent Care Visit
Setting: Outpatient Urgent Care Clinic
Name: Cody James Age: 11-year-old Gender: M Ethnicity: Caucasian
Reason for Visit: Acute right wrist pain following a soccer injury
Date of visit:
Vital Signs:
BP 106/70 mmHg; Respirations 18/min; Pulse 110 /min, Temperature 37.3°C (99.1°F), Height 4’8”; Weight 40 kg (88 lbs); BMI 19.7
HPI
Patient is an 11-year-old boy who presents to the urgent care with his parents due to acute right wrist pain following a fall during a soccer game about 1 hour ago. He collided with an opponent and landed on his outstretched right hand. He immediately experienced sharp pain in his wrist and digits and could not move his hand or wrist without severe pain. His parents noted swelling around his wrist and immediately brought him in for urgent evaluation.
His mother provides some general history about Cody and expressed concerns about his overall well-being. She reports that while Cody is still excited to play soccer, she has noticed that his skin color is pale, he appears more fatigued, and he is more short of breath with the same level of exertion that he has always been putting in. He is also getting sick frequently. She states that he “catches every cold or bug that goes around the classroom.” In addition to frequent respiratory infections, she also reports that he is having nosebleeds that are occurring both during his soccer games as well as in the middle of the night. Lastly, she noticed increasing bruising recently on his body but had attributed them to soccer and “rough housing” with friends. He lives at home with his parents and is only involved in soccer as his extracurricular activity outside of school.
History
Past Medical History
- ADHD
- Speech Language Impairment
Past Surgical History
- None
Family History
- Mother, 45 y/o - Hearing loss (uses assistive device)
- Father, 41 y/o -
- Sister, 14 y/o- Bulimia nervosa (recovered)
Social History
- No alcohol consumption
- No smoking
- No illicit drug use
- Lives at home with parents and sister
Medications and dosages the patient is currently taking:
None
Allergies - No Known Drug Allergies
Review of Systems
General: Positive for fatigue, pale appearance, and bruising easily. Denies recent infections other than common colds.
HEENT: Positive for frequent nosebleeds. No headaches or visual changes.
Respiratory: Positive for shortness of breath on exertion. No cough or wheezing.
Cardiovascular: No chest pain or palpitations.
Gastrointestinal: No nausea, vomiting, diarrhea, or abdominal pain.
Musculoskeletal: Positive for right wrist pain and swelling. No other joint pain or swelling.
Neurological: No seizures or changes in mental status.
Psychiatric: No anxiety or depression reported.
Physical Examination
General: Well-nourished, well-developed young male in mild distress due to pain. He appears pale and fatigued, sitting on the exam table.
HEENT: Normocephalic, atraumatic. Conjunctivae are pale, and sclerae are non-icteric. No signs of nasal trauma. Nasal mucosa without erythema or edema, no active bleeding from the bilateral nares. No foreign bodies or obvious sources of bleeding were visualized. The septum is midline without deviation or perforation. Turbinates are mildly enlarged bilaterally without signs of active bleeding, purulence, or crusting. Posterior pharynx without blood or erythema, no tonsillar hypertrophy, Oral mucosa moist.
Thyroid: No thyromegaly. No thyroid nodules are appreciated. No cervical lymphadenopathy.
Lungs:Clear to auscultation bilaterally in A/P lung fields.
CV: Regular rate and rhythm with no murmurs, rubs, gallops.
Abdomen: Soft, non-distended protuberant abdomen. No tenderness to palpation x 4 quadrants. Abdomen without varicosities, rashes, masses, hernias, or ascitic fluid. Normoactive bowel sounds x 4. There is no guarding or rigidity. No rebound tenderness to palpation. No CVA tenderness to palpation bilaterally.
Right hand:The skin of the right hand and all digits are intact, with no open wounds or sores. Nails are intact without cyanosis, cap refill < 2 seconds bilaterally upper and lower extremities. Ecchymosis and edema are noted around the right proximal 3rd phalanx. Severe bony tenderness to palpation over the 3rd proximal phalanx. Limited active and passive range of motion of the 3rd proximal phalanx secondary to pain. Unable to fully flex or extend the 3rd proximal phalanx. All other digits have intact skin, without tenderness to palpation, and there is full active and passive range of motion of the digits.
Right Wrist: The skin of the right wrist is intact, with no open wounds or sores. No deformity is appreciated. There is no tenderness to palpation over the ulnar or styloid processes. There is no anatomical snuff box tenderness.
Left hand: The skin of the left hand and all digits are intact, with no open wounds or sores. Nails are intact without cyanosis, cap refill < 2 seconds—non-tender to palpation, full active and passive range of motion of the digits in all planes.
Left Wrist: The skin of the left wrist is intact, with no open wounds or sores. No deformity is appreciated. There is no tenderness to palpation over the ulnar or styloid processes. There is no anatomical snuff box tenderness.
Skin: Multiple ecchymoses scattered throughout bilateral lower extremities in various stages of healing. There are no linear loop marks, skin burns, or handprints on the body.
Right Shoulder: There is mild elevation of the lateral clavicle without skin tenting compared to the left shoulder. Palpation of the AC joint reveals significant point tenderness at the AC joint. There is no crepitus on palpation. No tenderness to palpation of the biceps tendon, coracoid, or subacromial space. The arm is held flexed at 90 degrees. There is a limited active range of motion with significant pain and limitation with abduction, flexion, and extension. Negative Neer’s test, negative drop arm test. Positive Scarf test and cross-arm test.
Left shoulder: No clavicle deformity is appreciated. There is no tenderness to the AC joint, biceps tendon, coracoid, or subacromial space palpation. There is full active and passive range of motion without pain in forward flexion, abduction, adduction, external rotation, and internal rotation. Negative Neer’s test, negative drop arm test, negative scarf test, negative cross arm test.
Neurovascular: Distal sensation and motor function in the right upper extremity are intact. Pulses at the radial and brachial arteries are palpable and equal bilaterally.
Diagnostics:
LABORATORY RESULTS:
CBC
| CBC w/ diff | Test Result | Reference Range |
| WBC | 25 | 3.9 – 11.1 |
| RBC | 3.9 | 4.2 – 5.7 |
| Hgb | 14.5 | 13.2 – 16.9 |
| Hct | 43.5 | 38.5 – 49.0 |
| MCV | 91 | 80 - 97 |
| MCH | 31.6 | 27.5 - 33.5 |
| MCHC | 33.1 | 32.0 - 36.0 |
| Platelet | 110 | 140 - 390 |
| RDW - CV | 12.7 | 11.0 - 15.0 |
| MPV | 10.3 | 9.6 - 12.0 |
| Bands | 2 | 0-3 |
| Neutrophils % | 63 | 50 - 70 |
| Lymphocytes % | 28 | 20 - 40 |
| Monocytes % | 2 | 2 - 8 |
| Eosinophils % | 3 | 1 - 4 |
| Basophils % | 1 | 0 - 1 |
Right hand and wrist X-ray

Radiologist interpretation: Fracture extends through the growth plate (physis) and into the metaphysis. The epiphysis appears intact with no involvement in the fracture. There is soft tissue swelling present around the site of the fracture, correlate clinically.
Conclusion: Right proximal middle finger Salter-Harris II fracture with mild displacement and no significant angulation.
R shoulder X-ray: AC separation, aka sprain

Radiologist interpretation: No fracture is identified. The right acromioclavicular joint is disrupted, with elevation of the clavicle with respect to the acromion. Coracoclavicular distance is also increased. Features are those of a left grade III acromioclavicular joint injury.
-
Assessment and Plan
-
Right proximal middle phalanx Salter-Harris II fracture
-
Aluminum finger splint applied on the right middle phalanx as well as a short arm splint was placed in the office to immobilize the wrist. The patient tolerated the procedure well. Patient and family understand return precautions and should call if experiencing any of the following: Numbness/tingling in fingers, persistent pain, swelling or discoloration of the extremities or fingers. When showering, avoid getting the splint wet, and wrap it in the protective bag. Do not place sharp objects, such as pens or forks, inside the splint if it becomes itchy. This is to avoid causing potential skin injury.
- Pain control was discussed, and RX was sent for Ibuprofen 400 mg q4 hours with food as needed for pain control.
- Referral to orthopedics will be placed ASAP for further monitoring and possible cast application.
- Follow up with orthopedics within one week.
-
Aluminum finger splint applied on the right middle phalanx as well as a short arm splint was placed in the office to immobilize the wrist. The patient tolerated the procedure well. Patient and family understand return precautions and should call if experiencing any of the following: Numbness/tingling in fingers, persistent pain, swelling or discoloration of the extremities or fingers. When showering, avoid getting the splint wet, and wrap it in the protective bag. Do not place sharp objects, such as pens or forks, inside the splint if it becomes itchy. This is to avoid causing potential skin injury.
-
Grade 2 acromioclavicular sprain, Right shoulder
-
Placed in a sling immobilizer today and will need to follow up with Orthopedics within one week. An orthopedics referral will be placed today. Do not: Ignore any worsening pain, swelling, or redness around the injured joint. Contact your doctor if you experience these symptoms. Advised to:
- Rest and avoid strenuous activity that can aggravate the injury. Avoid overhead, pulling, pushing, lifting, and contact sports.
- Ice: Apply ice packs wrapped in a towel to the affected area for 15-20 minutes at a time, several times a day. Do not apply ice directly to your skin.
- Compression: You might be fitted with a sling to immobilize your shoulder and reduce pain. Wear the sling as directed by your doctor, typically for a few hours at a time or only when needed for pain relief.
- Elevation: Elevate your injured shoulder above your heart whenever possible to reduce swelling.
-
Placed in a sling immobilizer today and will need to follow up with Orthopedics within one week. An orthopedics referral will be placed today. Do not: Ignore any worsening pain, swelling, or redness around the injured joint. Contact your doctor if you experience these symptoms. Advised to:
-
Fatigue
- CBC in-house concerning possible blood dyscrasia, especially in the context of other abnormal lab findings that the patient demonstrated on CBC, including leukocytosis, erythrocytopenia, and thrombocytopenia. It was recommended that the mother contact his pediatrician for a stat referral to hematology for further investigation and workup of lab abnormalities and concerning symptomatology.
- Leukocytosis: See Above: Requires referral from Pediatrician to see Peds Oncology
- Thrombocytopenia: See Above: Requires referral from Pediatrician to see Peds Oncology
- Erythrocytopenia, See Above: Requires referral from Pediatrician to see Peds Oncology.
-
Bruising with minimal to no trauma
- Bruising is confined solely to bilateral lower extremities. Discussion with mother on abuse risk factors, which is found to be an unlikely cause due to no previous history of fractures or injuries, patient lives at home with his parents and is not watched by any adults other than his parents. In the office, he shows no signs of fearful behavior. Advised mother to continue monitoring for new bruise development and inquire if any known fall or injury occurred to that area.
-
Frequent Nosebleeds
- Nasal exam without abnormality or foreign body. Consider frequent URIs and/or allergic causes. Avoid picking your nose. You may apply lubricant, such as Aquaphor, to the nasal canal to prevent dryness.
-
Frequent URIs
- Follow up with his pediatrician and ensure compliance with all age-appropriate vaccines. Consider immunology evaluation given frequent illness history and discuss the benefits of frequent hand washing and using a mask when others are sick.
-
Right proximal middle phalanx Salter-Harris II fracture
Providers Signature: Penelope Woods PA-C
Physician/PA Follow Up

Cody James Pediatric Visit
Setting: Outpatient Urgent Care Clinic
Name: Cody James Age: 11-year-old Gender: M Ethnicity: Caucasian
Reason for Visit: Acute right wrist pain following a soccer injury
Date of visit:
Vital Signs:
BP 112/72mmHg; Respirations 18/min; Pulse 105 /min, Temperature 36.9°C (98.4°F), Height 4’8”; Weight 40 kg (88 lbs); BMI 19.7
HPI
Cody is an 11-year-old male patient with a diagnosis of Acute Lymphoblastic Leukemia (ALL), who presents today for a one-month follow-up since starting chemotherapy. Cody began chemotherapy about ten days after his ALL diagnosis, under the care of the pediatric oncology team.
Since starting chemotherapy, Cody has been closely monitored by his oncologist. The serial laboratory results his oncologist has been tracking demonstrates a positive response to treatment with expected improvements in clinical markers. However, Cody has been experiencing significant fatigue and muscle weakness. His parents have observed a noticeable decline in energy levels including no longer engaging in physical activities with friends. His parents have opted to homeschool him due to concerns about his increased susceptibility to infections. Both parents have observed that his stutter has become more pronounced since being homeschooled. Cody is consistently repeating initial sounds like "C-c-can I have a p-p-piece of paper?" He will also perform whole word repetition such as "Can-can I go to the b-bathroom?" and syllable repetition as in "I-I-I want to play soccer.”
Recently, Cody sustained a right middle finger fracture and an AC sprain of his right shoulder. He has already been seen, and treated, by orthopedics and his mother states that he is improving.
In addition to the current symptoms, Cody has a history of Attention Deficit Hyperactivity Disorder (ADHD). His ADHD has made it challenging for him to stay focused on his schoolwork, especially since he had difficulty with completing handwritten tasks after his finger injury.
His oncologist recommended Cody be seen today for further evaluation and management of his symptoms. His mother happily reports that Cody has not contracted any recent colds or viruses. He also has not had any recent nosebleeds.
History
Past Medical History
- Acute Lymphocytic Leukemia (ALL)
- ADHD
- Speech Language Impairment
- Right proximal middle phalanx Salter-Harris II fracture
- Grade 2 acromioclavicular sprain, right shoulder
- Fatigue
- Leukocytosis
- Thrombocytopenia
- Erythrocytopenia
- Recurrent nosebleeds
- Frequent upper respiratory infections
Current Medications and Dosages
- None
Past Surgical History
- None
Family History
- Mother, 45 y/o - Hearing loss (uses assistive device)
- Father, 41 y/o -
- Sister, 14 y/o- Bulimia nervosa (recovered)
Social History
- No alcohol consumption
- No smoking
- No illicit drug use
- Lives at home with parents and sister
Allergies - No Known Drug Allergies
Review of Systems
General: Positive for fatigue, pale appearance, and bruising easily. Denies recent infections.
HEENT: Negative for nosebleeds. No headaches or visual changes.
Respiratory: No shortness of breath on exertion. No cough or wheezing.
Cardiovascular: No chest pain or palpitations.
Gastrointestinal: No nausea, vomiting, diarrhea, or abdominal pain.
Musculoskeletal: Stiffness of right wrist and right shoulder. No other joint pain or swelling.
Neurological: No seizures or changes in mental status.
Psychiatric: No anxiety or depression reported.
Physical Examination
General: Well-nourished, well-developed young male in no distress. He appears pale and fatigued, sitting on the exam table.
HEENT: Normocephalic, atraumatic. Conjunctivae are pale bilaterally, and sclerae are non-icteric. Nasal mucosa without erythema or edema, no active bleeding from the bilateral nares. Posterior pharynx without blood or erythema, no tonsillar hypertrophy, Oral mucosa moist.
Thyroid: No thyromegaly. No thyroid nodules appreciated. No cervical lymphadenopathy.
Lungs:Clear to auscultation bilaterally in A/P lung fields.
CV: Regular rate and rhythm with no murmurs, rubs, gallops.
Abdomen: Soft, non-distended abdomen. No tenderness to palpation x 4 quadrants. No CVA tenderness to palpation bilaterally.
Right hand:Nails are intact without cyanosis, cap refill < 2 seconds bilaterally. No bony tenderness, erythema, or edema of the 3rd middle phalanx. Slight decrease in ROM of the third middle phalanx with extension. Full active and passive ROM of all other digits.
Right Wrist: No deformity is appreciated. There is no tenderness to palpation over the ulnar or styloid processes. Mild limitation in active and passive range of motion of the joint, most noticeable during supination and pronation and at the extremes of flexion and extension. No pain with ulnar or radial deviation. There is no anatomical snuff box tenderness.
Left hand: The skin of the left hand and all digits are intact, with no open wounds or sores. Nails are intact without cyanosis, cap refill < 2 seconds—non-tender to palpation, full active and passive range of motion of the digits in all planes.
Left Wrist: No deformity is appreciated. There is no tenderness to palpation over the ulnar or styloid processes. Full active and passive range of motion of the joint. There is no anatomical snuff box tenderness.
Skin: No ecchymosis appreciated.
Right Shoulder: There is no deformity present compared to the left shoulder. Palpation of the AC joint reveals no tenderness. There is no crepitus on palpation. No tenderness to palpation of the biceps tendon, coracoid, or subacromial space. There is a limited active range of motion with flexion and extension. Negative Neer’s test, negative drop arm test. Negative scarf test and cross-arm test.
Left shoulder: No clavicle deformity is appreciated. There is no tenderness to the AC joint, biceps tendon, coracoid, or subacromial space palpation. There is full active and passive range of motion without pain in forward flexion, abduction, adduction, external rotation, and internal rotation.
Neurovascular: Distal sensation and motor function in the right upper extremity are intact. Pulses at the radial and brachial arteries are palpable and equal bilaterally.
In house diagnostics:
-
Acute Lymphocytic Leukemia (ALL)
- Continue follow up with Peds Oncology to monitor response to chemotherapy with routine blood work and management of side effects of chemotherapy.
- Request progress notes from Peds Oncology office to update patient’s medications.
-
Fatigue:
- Suspect that this is a side effect from chemotherapy. Consider diagnosis to include comorbid depression given recent cancer diagnosis.
- Referral to Physical Therapy: For evaluation and management of cancer-related fatigue. Physical therapy can help with energy.
- Energy Management: Educate the patient and caregivers on managing energy levels, including rest periods and pacing activities.
-
Nutritional Support:
- Balanced Diet: Ensure the patient consumes a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to maintain energy levels.
- Small, Frequent Meals: Encourage small, frequent meals and snacks to avoid energy dips.
- Hydration: Maintain adequate hydration, aiming for at least 8 cups of water per day, unless otherwise advised by a healthcare provider.
-
Sleep Hygiene: Promote good sleep hygiene practices, such as:
- Keeping a regular sleep schedule.
- Creating a restful sleep environment (cool, dark, and quiet).
- Avoiding caffeine and electronic devices before bedtime.
- Rest Periods: Encourage short naps or rest periods during the day, but avoid long naps that can interfere with nighttime sleep.
-
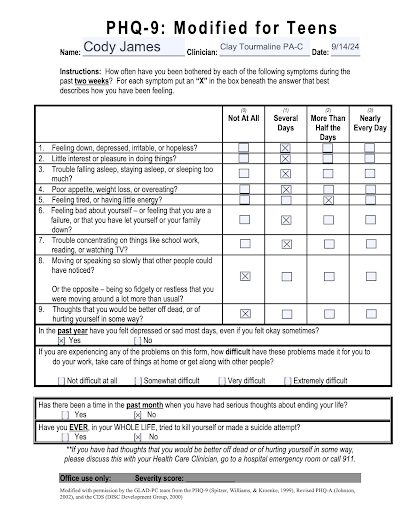
Mild Depression:
- PHQ9 Modified for Teens- Scored 9, equating to mild depression.
- Referral to Behavioral Health for evaluation and talk therapy
- Patient appears to be having difficult transition to new life circumstances, including cancer diagnosis, injury to right hand and shoulder, homeschooling, and familial financial struggle.
- No Suicidal/homicidal ideation, parents to monitor symptoms
-
ADHD
- Potential exacerbation in light of change from in person schooling with IEP to homeschooling after cancer diagnosis.
- Referral to Behavioral Health for possible CBT/behavior modification assistance. Possible benefits:
- Helps children with ADHD develop problem-solving skills, manage impulsive behaviors, and improve their emotional regulation.
- CBT can also address co-occurring issues such as anxiety and depression.
-
Speech Language Impairment: Worsening during homeschooling:
-
Referral to Speech Language Pathologist for specialized therapy
- Education for Family and Friends: Educate family members and friends about stuttering to foster a supportive environment. Encourage patience and active listening without interrupting or finishing sentences.
- Adaptive Communication: Use of non-verbal communication methods such as gestures, writing, or using technology to assist communication when necessary.
-
Referral to Speech Language Pathologist for specialized therapy
-
Right wrist pain: Status post fall on outstretched hand. Patient still having stiffness with everyday use, suspect ligamentous sprain after injury.
- Referral to Occupational Therapy for gross motor strength evaluation after middle phalanx fracture. Continue to follow up with all planned orthopedic appointments.
-
Grade 2 acromioclavicular sprain, right shoulder:
- Cleared by Orthopedics to return to activity as tolerated, in-office patient has continued stiffness in the shoulder.
- Physical Therapy: Referral for physical therapy to improve shoulder strength and function, and to develop a rehabilitation plan.
- At home activities: Range of Motion Exercises: Gentle passive range of motion exercises to maintain mobility without stressing the AC joint.
- Pendulum exercises
- Gentle shoulder shrugs and scapular retractions
- Activity Modification: Avoid activities that may aggravate the injury until full recovery.
- Frequent nosebleeds: Mother reports no recent episodes of nosebleeding, continue to monitor.
-
Frequent upper respiratory infections
- Frequent handwashing and masking
- Up to date with all age appropriate vaccinations: Vaccinations are often scheduled during periods when the child’s immune system is more robust, typically during maintenance phases of chemotherapy or after completion of treatment.
- Discuss PPSV23 vaccine with Peds Oncology
Providers Signature: Clay Tourmaline PA-C
Athletic Trainer Note
Athletic Training Note
James, Cody
R AC, shoulder
R Wrist/hand
S: 11-yr old male, club soccer player; hx of ADHD; speech language impairment; high WBC count; ran into opponent; FOOSH on R hand; presents with following:
- Sharp pain at wrist and fingers
- Removed from play
- Severe pain with flex/exten of wrist and fingers
- Edema noted immediately
- Pain noted in R AC area of shoulder (secondary to wrist)
- Pain with R shoulder flexion noted during wrist x-ray
O: edema noted on the R wrist and fingers; piano key sign noted on AC joint
A: (+) cross over arm test
(+) Obrien’s test
X-ray results (+) piano key sign for Grade II AC sprain
X-ray results (+) R proximal 3rd finger Salter-Harris II fracture (casted)
P: follow up with pediatrician; follow up with OT for wrist/finger cast; follow up and care plan for AC sprain (refer to AT for RTP guidelines); follow up with oncologist
Follow-up notes:
S: 11-yr old patient Cody history of leukemia and doing Chemotherapy for several months; mother suspects signs of bulimia (frequent bathroom visits after eating large meals) in daughter; Daughter (Kelly) seems to retreat when attention given to brother Cody; severe tooth and mouth pain
O: denies bulimia (emotional)
A: mouth pain and tooth pain; mouth ulcer
P: create care plan for Cody
Audiology Note
Audiology Chart Notes
PATIENT: Kristi James
DATE OF VISIT: (2 months before Cody’s accident)
Kristi was seen today for a routine 6-month check for her Phonak Audeo receiver-in-the canal hearing aids. She reported that the hearing aids seem to be working well and she has no trouble keeping them clean. She noted that she uses a headset for work and sometimes forgets to put her hearing aids back in when she takes the headset off. She said that she hears well with the headset and reported no concerns hearing at work. She reported that forgetting to put her hearing aids back in after work causes difficulty for her on occasion. One example of this is struggling to hear if the family goes out for the evening and she has left the hearing aids at home. She reported that on occasion she forgets to put her hearing aids in even on days where she does not use the headset.
The hearing aids appear to be well-maintained and in good working order. Datalogging indicates intermittent hearing aid use with average daily use of 2 hours over the past 6 months.
When asked, Kristi said she felt it would be most beneficial to talk about how she forgets to put her hearing aids in. This was the focus of today’s visit. She said that she would like to wear them more often but has struggled developing a habit of putting them in, even though she has been wearing them for 2 years. She noted that she was embarrassed about this and felt she should be better at wearing her hearing aids by now. She also said she was frustrated about having one more thing to keep track of in her sometimes-hectic life. She said that she does hear better with them in and does not have complaints or concerns about physical comfort or benefit of the hearing aids.
I reassured Kristi that it is ok if it takes a long time to develop a habit and feelings of frustration are normal. I invited her to tell me more about how she feels and she spent some time sharing about difficulties balancing work and home life with two school-age children. I asked if she would like help figuring out how to develop the habit of wearing her hearing aids and she said that she would appreciate that. To start, I asked her to tell me about ways she had been successful in developing new habits in the past. After some discussion and considering different strategies, she determined that setting a reminder in her phone would be the best thing to try first. I offered to send her scheduled reminder e-mails and she said she would like to receive weekly reminder e-mails every Monday mid-morning for one month.
Plan: Follow up in 3 months or sooner as needed. Weekly reminder e-mails scheduled in secure messaging system.
DATE OF VISIT: (1 month after Cody’s accident)
Patient postponed follow-up appointment via voicemail message. She noted some family struggles and health concerns regarding her son and requested a 3-month postponement. Note made to contact her in 2 months to schedule a follow-up.
Dental Note
Dental Notes for Cody James
Patient: Cody James, an 11-year-old male, presented to a dental office with a Chief Complaint of susceptible gums, pain upon chewing, and bleeding.
Medical History: Medical History (Based on Summarized Narrative): Two weeks ago, while playing a fast-paced game of soccer, Cody ran headlong into a member of the opposing team, falling on his outstretched right hand. He immediately experienced sharp pain in the digits and wrist and was taken off the field and into the care of his parents. Cody couldn’t move his hand and wrist without severe pain, and as the parents noticed that it was beginning to swell, they decided to take him to the pediatric urgent care center since it was Saturday, and his pediatrician wasn’t available.
Upon arrival at the Urgent Care, Cody was taken to Radiology, and after the x-ray, a CBC was obtained. The x-ray results were reviewed, and a right proximal middle finger Salter-Harris II fracture was identified. Also identified was a Grade 2 acromioclavicular sprain (slight elevation of the lateral clavicle), which was noted through a shoulder x-ray, which was ordered when Cody experienced pain with lifting his arm for the arm/wrist x-ray. The hand and wrist were splinted, and a follow-up appointment was made with Cody’s pediatrician in 3 days. Additionally, Cody was referred to physical therapy or his athletic trainer to manage the shoulder injury. The blood test revealed a higher-than-normal white cell count and reduced levels of platelets and red blood cells.
Cody had an appointment with his pediatrician within the week, who referred him to pediatric oncology. The oncologist ordered a bone marrow biopsy, which confirmed the diagnosis of acute lymphocytic leukemia (ALL). The same week, Cody began chemotherapy at the local cancer center with a pediatric oncologist directing his care, which was expected to continue over the next 2-3 years.
Cody’s emotional state was affected as he worried about the impact of his injury on his soccer engagements. Financial concerns about hospital bills and treatment expenses also weighed on his mind.
Diagnosis:
Based on confirmed acute lymphocytic leukemia, the dental examination and radiographic findings further explored the effects of ALL on the oral cavity and surrounding structures.
Dental Examination and Treatment Recommendations (Incorporating Pediatric Oncology Information):
The patient had a mild fever of 103.1 F with a heart rate of 134 beats per minute. Extraoral examination revealed painless bilateral lymphadenopathy below the mandibular angle. Intraoral examination observed no salivary gland swelling and revealed buccal mucosa pallor with well-demarcated, painless, soft, bilateral maxillary gingival overgrowth. Significant bleeding of the gingival tissues was observed upon palpation. The exam noted mobility of the mandibular primary molars. The dentist requested a panoramic film and bitewings. Upon obtaining consent from Mrs. James, the panoramic and a full series of X-rays were taken. Both radiographic exams showed no specific signs of dental infection contributing to the patient’s condition, and although the mandibular primary molars had minimal mobility, radiographic evaluation of the periodontal ligament space did not show enlargement for these or other teeth. These images are a valuable baseline for assessing oral conditions during cancer therapy. Primary mandibular molars had occlusal caries.
The dentist called the patient’s pediatric oncologist to obtain blood work results and find the status of Cody's treatment. The dentist received Cody’s latest blood test, which revealed:
Severe anemia (low hemoglobin, 11.2 grams/dl; average values 13.2 to 16.6 grams/dl), thrombocytopenia (low platelet count, 45,000 platelets/mcL; average values 150,000-300,00 mcL), and leukopenia (low white blood cell count, 600 per microliter; average value 5,000 to 10,000 per microliter). Initially, the patient went into a rapid phase of induction chemotherapy to achieve remission. The patient received three medications: L-asparaginase, vincristine, and dexamethasone, each given during the first month. It is highly recommended that patients receive a comprehensive oral exam before starting chemotherapy.
- Dental findings included Mouth ulcers, gingival abnormalities, petechiae, and spontaneous bleeding. Both lower primary molars exhibited small caries lesions that must be addressed ASAP.
- Oral mucosa is susceptible, with multiple ulcers, omnipresent candida infection signs, and slightly dry mucosa.
- Management of oral infections and pain: Provide appropriate pain management strategies to alleviate his discomfort and to eliminate mucositis and candida infection.
The following medications may be prescribed for Cody James based on the presented case:
Diphenhydramine 0.075%
Hydrocortisone 0.125%
Nystatin 100,000 U/ml (units/milliliter)
Mix and dispense 30 milliliters (ml) of nystatin suspension at 100,000 U/ml or 3 million units of nystatin powder with 60 milligrams of hydrocortisone and diphenhydramine HCL syrup to bring the total volume to 240 ml.
Antibiotics: In cases of orofacial infections, antibiotics may be prescribed to prevent or manage potential infections. Commonly used antibiotics for dental infections include Amoxicillin or Clindamycin. However, it's essential to consider the patient's allergies and any drug interactions before prescribing antibiotics.
Prescription Pain Medication: In cases of severe pain that cannot be effectively managed with over-the-counter analgesics, a short-term prescription for potent pain medication, such as Hydrocodone or Oxycodone, may be considered. However, these medications should be used judiciously, as they carry a risk of dependence and should only be used when necessary and under close supervision.
Topical Anesthetics: Topical numbing gels, like Benzocaine, can temporarily relieve localized oral pain, mainly if there are oral mucosal injuries or irritation.
Mouthwash or Oral Rinse: An alcohol-free antimicrobial mouthwash or oral rinse may be recommended to help maintain oral hygiene and prevent infection in the affected area.
It is essential to carefully assess the patient's medical history, current medications, and any allergies before prescribing any medications. Additionally, patient education should be emphasized, explaining the proper usage, potential side effects, and adherence to prescribed medication regimens.
Dietary restrictions for Cody James following chemotherapy the following recommendations may be suggested:
Soft Diet: Initially, Cody James should adhere to a soft diet to avoid putting excessive pressure on the injured area. Foods that require minimal chewing, such as soups, mashed potatoes, yogurt, smoothies, and soft fruits, can be included in his diet.
Hard and crunchy foods, like nuts and chips, should be avoided to prevent additional mucosal irritation.
Limit Acidic Foods and Beverages: Acidic foods and drinks, such as citrus fruits and carbonated beverages, can irritate oral tissues and affect healing. It's advisable to limit their consumption.
Hydration: Encourage the patient to maintain proper hydration by drinking plenty of water throughout the day. Staying hydrated is essential for overall health and aids in the healing process. Frequent sips of the water will help with dry mouth.
Follow Dentist's Recommendations: Based on his case and treatment plan, Cody James should follow any specific dietary recommendations provided by the dentist or his medical team.
Follow-up:
The frequency and duration of follow-up visits may vary based on the severity of the injury and the specific treatment interventions. However, a general guideline for follow-up visits may include:
- Initial Follow-up (within a week): Schedule an initial follow-up appointment within a week of the initial dental visit to excavate all caries lesions, if possible, put permanent composite restorations on caries-affected primary molars, and check for any signs of oral infection or complications. Evaluation of mucosal healing and reduction of candida infection should also be performed.
- Subsequent Follow-ups (as needed): Depending on the patient's progress and response to treatment, subsequent follow-up visits may be scheduled every few weeks or as determined by the dentist. These visits will allow for ongoing monitoring of oral condition and any signs of infection.
- Regular Check-ups: Cody James should continue with regular dental check-ups and cleanings, typically scheduled every six months following the initial healing period. These routine appointments will help maintain oral health and detect potential issues early on.
Patient Education: Patient education on proper oral hygiene practices and adherence to dietary restrictions should be reinforced during follow-up appointments. Additionally, encouraging open communication with the patient about any concerns or changes in symptoms will help ensure that Cody James receives comprehensive care and support throughout his recovery.
Prognosis: The prognosis for Cody James’ dental condition will depend on his compliance with the prescribed treatment plan, emotional well-being, and his overall response to cancer treatment.
Occupational Therapy Note
Pt is a right hand dominant 11 y/o male who sustained a right middle finger proximal phalanx Salter-Harris II fracture post fall on outstretched hand while playing soccer.
Pt was referred to OT for evaluation and treatment 1-2x/week for 6 weeks. Pt is 6 weeks post fracture with no limitations for therapy on ROM/strength as fracture is well healed.
S: Pt and parent report that pt has difficulty with writing, tying shoes, and brushing teeth due to decreased right middle finger ROM. Pt and parent report difficulty with gripping and pulling handles (car door, refrigerator) and opening drink bottles/snack packages due to decreased ROM and strength.
O: Pt accompanied by parent during OT evaluation in outpatient clinic x 60 minutes.
ROM:
| Digit | Left Hand ROM (Degrees) extension/flexion | Right Hand ROM (Degrees) extension/flexion |
| Thumb | WNL | WNL |
| Index | WNL | WNL |
| Middle | ||
| MCP | WNL | 10/60 |
| PIP | WNL | 35/60 |
| DIP | WNL | 10/40 |
| Ring | WNL | WNL |
| Small | WNL | WNL |
| Left | Right | |
| Wrist | ||
| Flexion | WNL | WNL |
| Extension | WNL | WNL |
| Radial deviation | WNL | WNL |
| Ulnar deviation | WNL | WNL |
| Forearm | ||
| Supination | WNL | WNL |
| Pronation | WNL | WNL |
| Elbow | ||
| Flexion | WNL | WNL |
| Extension | WNL | WNL |
Pt’s shoulder is being evaluated by physical therapy. Pt presents with decreased Right shoulder AROM.
Strength:
| Left hand | Right hand | |
| Grip (dynamometer rung II) | 35 lbs | 12 lbs |
| Lateral pinch | 13 lbs | 6 lbs |
| 2 point pinch | 8 lbs | 3 lbs |
| 3 point pinch | 8 lbs | 3 lbs |
Fine Motor Coordination:
9 hole peg test
| Left hand | Right hand |
| 40 seconds | 55 seconds |
Gross Motor Coordination:
Box and Blocks assessment
| Left hand | Right hand |
| 45 blocks | 30 blocks |
Sensation:
Pt denies numbness and tingling in bilateral hands. Light touch screening of bilateral upper extremities normal.
Edema (circumferential measurement):
| Left middle finger proximal phalanx | Right middle finger proximal phalanx |
| 4 cm | 4.5 cm |
ADLs:
| Activity | Assistance Level |
| Upper body dressing | Independent with donning/doffing t-shirts |
| Lower body dressing | Minimal assist with fastening buttons/zippers, Moderate assist with tying shoes |
| Grooming | Modified independence with brushing teeth due to increased time required/difficulty gripping |
| Bathing | Minimal assistance. Difficulty with squeezing shampoo bottles to dispense product. |
| Self-feeding | Moderate assistance. Difficulty with cutting food with a knife, opening refrigerator door, opening snack packaging, opening drink bottle caps |
IADLs:
| Activity | Limitations |
| School | Pt experiences difficulty with grasping pencil to write due to decreased Right middle finger ROM. Pt is able to type on keyboard, requires increased time. |
| Social participation | Pt’s in-person social participation with friends has decreased since diagnosis of CA. Pt socializes with friends via text and social media, however reports feeling lonely. |
| Caring for others | Prior to injury, pt fed and walked the family dog. He has not participated in these activities since injury. |
A: Pt presents with decreased right middle finger ROM, grip and pinch strength, and coordination which is decreasing his ability to perform writing, dressing, grooming, bathing, and self-feeding independently. Pt would benefit from continued skilled occupational therapy to increase his right middle finger ROM, grip/pinch strength, and coordination in order to increase his independence with ADLs/IADLs.
P: Continue OT 1-2x/week x 6 weeks for ROM, strengthening, ADL/IADL training/simulation, and modalities.
Physical Therapy Note

PT Notes
Name: Cody James
Age: 11 years old
Occupation: 6th grader, Bush Elementary
Sex: male
Referring healthcare professional: Penelope Woods, PA-C
Date of Referral:
Date of PT evaluation:
S:
C/C: “I get tired easily, but I want to go back to playing soccer again.”
History:
Cody James is an 11-year old boy who was referred to physical therapy (PT) following diagnosis of acute lymphocytic leukemia. Chemotherapy treatment has been started and from the referral received, patient has been responding favorably with treatment. He is followed closely by his oncology team. Prior to cancer diagnosis, Cody fell and fractured his right proximal middle finger (Salter-Harris II fracture) with a grade 2 right acromioclavicular sprain. His right hand/wrist was immediately put into a splint. He is scheduled for an x-ray on the fractured site in 3 weeks. Cody has been diagnosed with ADHD and has an Individualized Education Plan (IEP) for speech language impairment (SLI) for stuttering. The patient has been playing soccer since first grade and his parents have been very supportive of his interest in the sport.
Patient already expressed extreme fatigue at the start of the evaluation and told PT that “I would like to go home now…..I don’t want to do anything.” Patient also reported discomfort in right shoulder area.
Social history:
- Lives with parents: Dad (Blake) is a maintenance technician at a local hospital while Mom (Kristi) is a virtual assistant
- Has a teenage sister (Kelly) who suffers from bulimia and has been seeking medical attention
- Mom has bilateral hearing impairment and uses bilateral hearing aids
- Dad has good health insurance coverage, although money has been tight lately
O:
V/S: BP – 110/80 mmHg
HR – 65 bpm
RR – 16 cpm
PR – 70 bpm
Ocular inspection:
- Patient appeared very fatigued while seated, had to rest head on Mom’s shoulder
- Finger splint in place (right wrist/hand); no visible discoloration of right finger nail beds
Manual Muscle Testing –right hand/wrist muscles not tested as patient strongly refused to participate in testing
Myotome Testing – not tested at this time, patient refused
Sensory Testing – was only able to test bilateral C2 to C5, grossly graded 2/2 (light touch and pin prick for pain). All other dermatomes not tested this time due to patient refusal
Range of motion: Except for right hand/wrist (not tested as still in splint), all other joints grossly graded full ROM; patient refused to participate in actual ROM measurement for all other joints
Muscle palpation – not tested due to patient refusal, but previous medical report noted tenderness over right acromioclavicular area
A:
PT Impression: generalized deconditioning secondary to chemotherapy treatment
Problem lists:
- Generalized fatigue secondary to chemotherapy treatment
- Anticipated* decreased ROM of right hand and wrist
- Anticipated* decreased ROM right shoulder secondary to acromioclavicular sprain
- Anticipated* decreased strength of right hand, wrist, and right shoulder muscles
- Anticipated* decrease in participation with PT sessions due to fatigue
*anticipated as baseline not established at this time due to patient’s refusal to participate in full evaluation of affected areas
P:
Short term:
- Gradually increase patient’s endurance level in between chemotherapy sessions to prevent further deconditioning – incorporate play activities and consider joint sessions with occupational therapist and/or speech-language pathologist
- Patient and family education re: monitoring of circulation on right hand (i.e. nail bed coloration) and prevention of further sprain right acromioclavicular joint
- Patient and family education regarding energy conservation techniques
Medium term:
- Address anticipated decreased range of motion in right hand and wrist
- Address anticipated decreased strength in right hand and wrist muscles
- Address anticipated decreased strength of right shoulder muscles
- Continue working on building patient’s endurance level
- Continue monitoring patient’s mental health (e.g. signs of depression) and refer to appropriate professional for further evaluation and management (e.g. psychologist)
Signed: John Doe, PT
Date
Public Health Note
Health Science/Public Health Education:
PATIENT/FAMILY EDUCATION AND SUPPORT NOTES
‘Pediatric Cancer Patient Educators’ Certified Health Education Specialists (CHES) in the Health Care setting may perform the following duties: Deliver and assess health education programs, coordination and outreach, enrollment and initial health assessments, motivate others to initiate behavior change, communicate/liaise with primary care physicians, hospitals and other health care providers, plan for health education interventions, translation of medical and health education material for dissemination to client/patient.
PATIENT/FAMILY EDUCATION AND SUPPORT NOTES: CHES
CHES can use the Resources to help provide patient/family education and recommendations
Public Health Resources for the family – to start with:
Health dept: https://www.maricopa.gov/5302/Public-Health
Federally Qualified Health Centers: https://carelistings.com/federally-qualified-health-centers/mesa-az
Community Mental Health Center: https://www.maricopa.gov/5043/Mental-Health-Substance-Use
Maricopa County: Maricopa Healthy App: https://health.maricopa.gov/app/
PATIENT/FAMILY EDUCATION FOR Acute lymphocytic leukemia
Give Education/Recommendation - Use Resources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5235950/
https://www.lls.org/sites/default/files/National/USA/Pdf/Publications/PS33_ALL_2018_final.pdf
https://www.cancer.gov/types/leukemia/patient/child-all-treatment-pdq
https://kidshealth.org/en/parents/all.html
https://leukemiarf.org/patients/
https://leukemiarf.org/patients/resources/children/
PATIENT/FAMILY EDUCATION FOR Financial Health/Health Insurance/Healthcare Resources
Give Education/Recommendation - Use Resources
Adelante Healthcare - Mesa: https://adelantehealthcare.com/locations/mesa/
Financial Literacy/Assistance - A New Leaf:
https://www.turnanewleaf.org/services/financial-empowerment/
https://www.turnanewleaf.org/services/financial-empowerment/financial-wellness/
MesaCAN: https://www.turnanewleaf.org/services/financial-empowerment/mesacan/
Hearing aid resources:
Adherence to using hearing aids:
https://ncbi.nlm.nih.gov/pmc/articles/PMC10138368/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4630952/
https://www.tandfonline.com/doi/full/10.3109/14992027.2016.1144240
Support for adherence: Brief Motivational Interviewing:
https://motivationalinterviewing.org/understanding-motivational-interviewing
https://knowledgeplus.nejm.org/wp-content/uploads/2023/10/motivational-interviewing.pdf
Assistance: https://www.mesaaz.gov/residents/limited-income-assistance-programs
PATIENT/FAMILY EDUCATION FOR homeschool groups
Give Education/Recommendation - Use Resources
https://www.thehomeschoolmom.com/homeschooling-in-arizona/homeschool-organizations-support-groups/
http://www.knowledgehouse.info/azhsgroups_maricopa.html
https://www.homeschoolinginarizona.com/
PATIENT/FAMILY EDUCATION FOR Mental Health
Give Education/Recommendation – Use Resources
Information for patient educators – bulimia - https://bulimiaguide.org/information_for_educators_coaches/
NEDA Toolkits – patient education - https://www.nationaleatingdisorders.org/toolkits/
Education – bulimia - https://www.mayoclinic.org/diseases-conditions/bulimia/diagnosis-treatment/drc-20353621
NIH – bulimia - https://www.nimh.nih.gov/health/topics/eating-disorders
NLM – bulimia - https://www.ncbi.nlm.nih.gov/books/NBK562178/
NEDA – bulimia - https://www.nationaleatingdisorders.org/bulimia-nervosa/
Treatment education - https://www.eatingdisorderhope.com/information
Sliding fee schedule clinics: https://www.azdhs.gov/prevention/health-systems-development/sliding-fee-schedule/index.php
Free MH services:
https://www.freementalhealthservices.org/ci/az-mesa
https://www.freeclinics.com/cit/az-mesa
Specialize – eating disorders:
https://www.psychologytoday.com/us/treatment-rehab/az/mesa?category=eating-disorders
https://www.nationaleatingdisorders.org/free-low-cost-support/
ADHD – CDC - https://www.cdc.gov/adhd/hcp/treatment-recommendations/index.html
ADHD support: https://www.psychologytoday.com/us/groups/az/maricopa-county?category=adhd
ADHD – patient education/treatment - https://www.uptodate.com/contents/treatment-of-attention-deficit-hyperactivity-disorder-in-children-beyond-the-basics
ADHD patient education/symptoms - https://www.uptodate.com/contents/1210#
Free materials - https://www.cdc.gov/adhd/communication-resources/index.html
Support for adherence: Brief Motivational Interviewing:
https://motivationalinterviewing.org/understanding-motivational-interviewing
https://knowledgeplus.nejm.org/wp-content/uploads/2023/10/motivational-interviewing.pdf
PATIENT/FAMILY EDUCATION FOR Light physical Activity
Give Education/Recommendation - Use Resource
Local YMCA has recreational and youth development programs on sliding fee scale: https://www.ymca.org/locations/east-valley-family-ymca
Speech-Language Pathology Note
Speech-Language Pathology Report
Client Name: Cody James
DOB:
Age: 11 years
Date of Report:
Background Information
Cody James is an 11-year-old male diagnosed with ADHD and Speech Language Impairment (SLI) related to stuttering. He attends Bush Elementary and is currently in the 6th grade, with an Individualized Education Plan (IEP) for his speech and language needs. Cody has been an active soccer player since first grade and participates in club soccer. Recently, Cody was diagnosed with acute lymphocytic leukemia and has been undergoing chemotherapy. Additionally, Cody's mother has a hearing impairment and wears hearing aids.
Assessment Information
Presenting Concern
Cody's fluency has been observed to decline, with increased stuttering occurrences, particularly since beginning chemotherapy. Stress from his medical condition, treatment, and subsequent lifestyle changes are likely contributing factors. Cody's speech disfluencies are characterized by:
- Sound repetitions (e.g., "C-c-can I have a p-p-piece of paper?")
- Whole word repetitions (e.g., "Can-can I go to the b-bathroom?")
- Syllable repetitions (e.g., "I-I-I want to play soccer")
Fluency and Stress
Fluency disorders such as stuttering can be exacerbated by stress. Cody's recent medical diagnosis and treatment regimen, combined with the physical and emotional stress of managing leukemia and its symptoms, have likely increased his anxiety levels. The familial stress, including his mother's hearing impairment and his sister's bulimia recurrence, further contribute to the overall stress within the home environment. These stressors may negatively impact Cody's speech fluency.
Relationship to Other Diagnoses
- Hearing Loss in the Family: Cody's mother's hearing impairment could indirectly affect Cody's stress levels. Communication difficulties and the added strain of managing Cody's health might contribute to an environment of heightened stress and anxiety for Cody.
- Speech Language Impairment (SLI): Cody’s pre-existing SLI makes him more susceptible to speech disfluencies under stress. His recent medical challenges, including chemotherapy-induced fatigue and muscle weakness, have compounded his difficulty in maintaining fluent speech.
Diagnosis
Based on the observed speech patterns and the impact of current stressors, Cody is diagnosed with mild to moderate stuttering. His stuttering is characterized by increased frequency and severity of sound, word, and syllable repetitions.
Recommendations
- Further Assessment: A comprehensive evaluation by a pediatric psychologist is recommended to assess the impact of stress and anxiety on Cody’s overall well-being and fluency. Additionally, re-evaluation by an audiologist is suggested to ensure optimal hearing support for his mother, reducing familial communication stress.
- Speech Therapy: Continued speech therapy focusing on fluency shaping and stress management techniques is essential. Therapy should aim to reduce stuttering severity and equip Cody with strategies to manage speech disfluencies in stressful situations.
- Counseling: Family counseling is recommended to address the emotional and psychological impact of Cody's diagnosis and treatment on the family dynamics. Support for Cody's sister, Kelly, should be included to manage her bulimia and to address feelings of neglect or stress.
- School Support: Given Cody’s homeschooling situation due to his medical condition, it is important to ensure that his educational needs, including accommodations for his ADHD and stuttering, are met. Coordination with his IEP team to update and implement necessary supports is crucial.
- Medical Coordination: Regular communication with Cody’s medical team, including his oncologist and pediatrician, is essential to monitor his overall health and its impact on his speech and language development.
Conclusion
Cody James presents with mild to moderate stuttering, likely exacerbated by the significant stress associated with his recent leukemia diagnosis and treatment. A multidisciplinary approach, including speech therapy, psychological support, and family counseling, is recommended to address his fluency issues and support his overall well-being.
Prepared by:
John Smith, M.S., CCC-SLP
Speech-Language Pathologist
Resources
Watch an example of a past team presentationWorkshop 1: Whole Person Healthcare
Workshop 2: Roles & Responsibilities
Workshop 3: Lived Experiences of a Cancer Survivor
Childhood Cancer Articles
Recent Advances in Treatment Options for Childhood Acute Lymphoblastic LeukemiaEnhancing Sibling Support in Oncology: Collaborative Care for Families Facing Cancer in Young People
Learn more about the roles and responsibilities of the care providers
Athletic trainers
Athletic Trainers use a medical based model to provide comprehensive patient care in the domains of prevention; clinical evaluation and diagnosis; immediate and emergency care; treatment and rehabilitation; and organization and professional health and well-being. Athletic Trainers are highly qualified, multi-skilled health care professionals who collaborate with physicians to provide total patient care. Athletic Trainers work under the direction of a physician as prescribed by state licensure statutes.
Audiologist
"An audiologist is a person who, by virtue of academic degree, clinical training, and license to practice is uniquely qualified to provide a comprehensive array of professional services related to the identification, diagnosis and treatment of persons with auditory and balance disorders, and the prevention of these impairments. Audiologists serve in a number of roles including primary service provider, clinician, therapist, teacher, consultant, researcher and administrator. In addition, the supervising audiologist maintains legal and ethical responsibility for all assigned audiology activities provided by audiology assistants and audiology students."
Source: Academy of Doctors of Audiology
Counselor
What is professional counseling?
“Counseling is a collaborative effort between the counselor and client. Professional counselors help clients identify goals and potential solutions to problems which cause emotional turmoil; seek to improve communication and coping skills; strengthen self-esteem; and promote behavior change and optimal mental health.”
Learn more at: https://www.counseling.org/mental-health-counseling/what-is-counseling
Dentist
What is a Dentist?
You will find an interesting article here about the important interconnection between oral health and systemic health. So don't forget the importance of collaborating with the dentist!
Doctor of osteopathic medicine
“Doctors of Osteopathic Medicine use a unique whole-person approach to help prevent illness and injury.
Accounting for approximately 11% of all physicians in the United States, Doctors of Osteopathic Medicine, or DOs, bring a unique, patient-centered approach to every specialty across the full spectrum of medicine. They are trained to listen and partner with their patients to help them get healthy and stay well.”
Learn more at: https://osteopathic.org/what-is-osteopathic-medicine/what-is-a-do/
Nursing:
Registered Nurses
“Registered nurses (RN) form the backbone of health care provision in the United States. RNs provide critical health care to the public wherever it is needed.
Key Responsibilities
- Perform physical exams and health histories before making critical decisions
- Provide health promotion, counseling and education
- Administer medications and other personalized interventions
- Coordinate care, in collaboration with a wide array of health care professionals”
Occupational therapist
Occupational therapy is the only profession that helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations). Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability.
Common occupational therapy interventions include helping children with disabilities to participate fully in school and social situations, helping people recovering from injury to regain skills, and providing supports for older adults experiencing physical and cognitive changes.
Occupational therapy practitioners have a holistic perspective, in which the focus is on adapting the environment and/or task to fit the person, and the person is an integral part of the therapy team. It is an evidence-based practice deeply rooted in science.
See also: https://www.aota.org/career/become-an-ot-ota/about-the-profession
Learn more at: AOTA.org
Physical therapist
Physical therapists are movement experts who optimize quality of life through prescribed exercise, hands-on care, and patient education. After making a diagnosis, physical therapists create personalized treatment plans that help their patients improve mobility, manage pain and other chronic conditions, recover from injury, and prevent future injury and chronic disease.
Physical therapists empower people to be active participants in their own treatment, and they work collaboratively with other health professionals to ensure patients receive comprehensive care. Physical Therapy entry-level educational programs are at the doctoral level with subsequent educational opportunities for fellowship and residency. Physical therapists work in a wide range of specialty areas for which they can obtain specialty certification e.g. acute care, aquatics, cardiovascular & pulmonary, geriatrics, home health, neurology, oncology, orthopedics, pediatrics, sports, and women's health.
See Also: https://www.apta.org/your-career/careers-in-physical-therapy/becoming-a-pt
Learn more at: apta.org
Physician assistant
What is a PA?
“PAs (physician associates/physician assistants) are licensed clinicians who practice medicine in every specialty and setting. Trusted, rigorously educated and trained healthcare professionals, PAs are dedicated to expanding access to care and transforming health and wellness through patient-centered, team-based medical practice.”
Learn more at: https://www.aapa.org/about/what-is-a-pa/
THE PUBLIC HEALTH EDUCATOR/PATIENT EDUCATOR’S ROLES AND RESPONSIBILITIES
PUBLIC HEALTH EDUCATION: CERTIFIED HEALTH EDUCATION SPECIALISTS [CHES]:
The U.S. Department of Labor – Bureau of Labor Statistics (BLS) has a classification of health educator and defines health educators (SOC 21-1091) as those that provide and manage health education programs that help individuals, families, and their communities maximize and maintain healthy lifestyles.Health Educators collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies, and environments.
They link health systems, health providers, insurers, and patients to address individual and population health needs. They may serve as resource to assist individuals, other health professionals, or the community, and may administer fiscal resources for health education programs.
Responsibilities/competencies of CHES
https://assets.speakcdn.com/assets/2251/hespa_competencies_and_sub-competencies_052020.pdf
- Area I: Assessment of Needs and Capacity
- Area II: Planning
- Area III: Implementation
- Area IV: Evaluation and Research
- Area V: Advocacy
- Area VI: Communication
- Area VII: Leadership and Management
- Area VIII: Ethics and Professionalism
CHES in healthcare
Individuals who hold the CHES® and MCHES® certifications have the versatility and skillsets to practice in many different career settings, across the country and even overseas. Job settings were identified in the Health Education Specialist Practice Analysis (HESPA) include the following: Community/non-profit, Healthcare/Hospitals, Government, School Health, Academia/Universities, and Business/Worksite. Job titles in the hospital and healthcare sector can vary. Some common titles include Community Benefits Manager, Outreach Manager, Patient Educator or Program Manager, Wellness Coordinator, and RN/Health Educator. Health Education Specialists in the Health Care setting may perform the following duties:
- Deliver and assess health education programs
- Coordination and outreach
- Enrollment and initial health assessments
- Motivate others to initiate behavior change
- Communicate/liaise with primary care physicians, hospitals and other health care providers
- Plan for health education interventions
- Translate of medical and health education material for dissemination to client/patient
Social worker
The profession of social work aims to improve functioning and overall well-being within individuals, families, organizations, and communities through change efforts. With a focus on the poor, the oppressed, and the vulnerable, social sciences such as sociology, psychology, political science, public health, economics, law, community and organizational change, are applied. Needs assessments are completed and interventions are planned to solve personal and social problems within client systems to enhance social change. Social work practice is often divided into three levels. Micro-work involves working directly with individuals and families, such as providing individual counseling/therapy or assisting a family in accessing services. Mezzo-work involves working with groups and communities, such as conducting group therapy or providing services for community agencies. Macro-work involves fostering change on a larger scale through advocacy, social policy, research development, nonprofit and public service administration, or working with government agencies. Professional training requires a master’s degree and most states require professional licensure. Social Workers are employed in a variety of settings including healthcare, government agencies education, corrections, public health, and public policy.
Source: Wikipedia
Speech language pathologist
Speech-language pathologists (SLPs) work to prevent, assess, diagnose, and treat speech, language, social communication, cognitive-communication, and swallowing disorders in children and adults.
Learn more at: https://www.asha.org/Students/Speech-Language-Pathology/
