Study Nasal MRSA Colonization in Dental Students
Contributors:
Ann Spolarich, RDH, PhD
Inder Makin, MD, PhD
Jolene Bowers, PhD
Michael Valentine, MS
David Engelthaler, PhD
Ann Spolarich, RDH, PhD
Inder Makin, MD, PhD
Jolene Bowers, PhD
Michael Valentine, MS
David Engelthaler, PhD
Participating Organizations:
Arizona School of Dentistry and Oral Health
Arizona School of Dentistry and Oral Health
Background
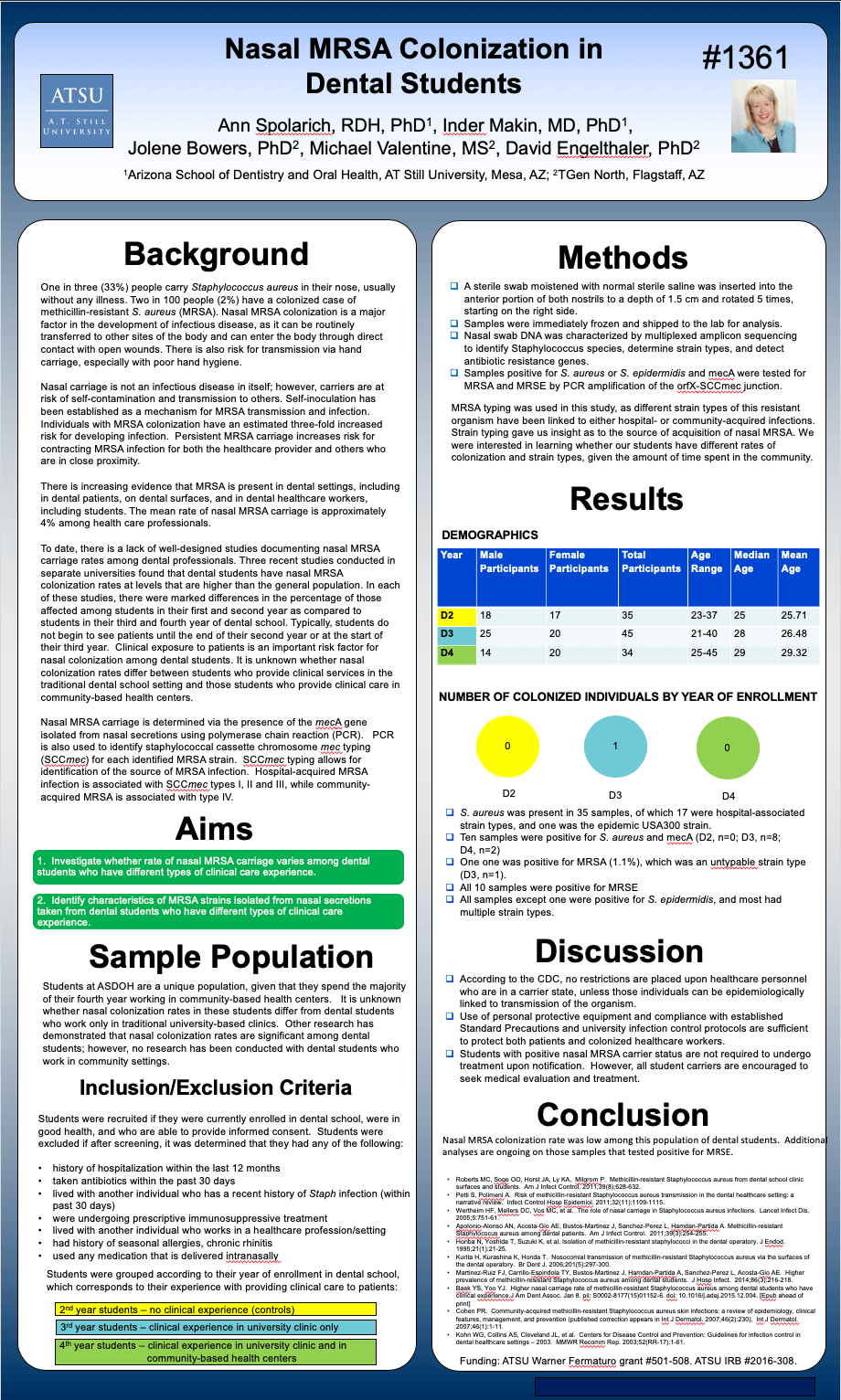
One in three (33%) people carry Staphylococcus aureus in their nose, usually without any illness. Two in 100 people (2%) have a colonized case of methicillin-resistant S. aureus (MRSA). Nasal MRSA colonization is a major factor in the development of infectious disease, as it can be routinely transferred to other sites of the body and can enter the body through direct contact with open wounds. There is also risk for transmission via hand carriage, especially with poor hand hygiene. Nasal carriage is not an infectious disease in itself; however, carriers are at risk of self-contamination and transmission to others. Self-inoculation has been established as a mechanism for MRSA transmission and infection. Individuals with MRSA colonization have an estimated three-fold increased risk for developing infection. Persistent MRSA carriage increases risk for contracting MRSA infection for both the healthcare provider and others who are in close proximity. There is increasing evidence that MRSA is present in dental settings, including in dental patients, on dental surfaces, and in dental healthcare workers, including students. The mean rate of nasal MRSA carriage is approximately 4% among health care professionals. To date, there is a lack of well-designed studies documenting nasal MRSA carriage rates among dental professionals. Three recent studies conducted in separate universities found that dental students have nasal MRSA colonization rates at levels that are higher than the general population. In each of these studies, there were marked differences in the percentage of those affected among students in their first and second year as compared to students in their third and fourth year of dental school. Typically, students do not begin to see patients until the end of their second year or at the start of their third year. Clinical exposure to patients is an important risk factor for nasal colonization among dental students. It is unknown whether nasal colonization rates differ between students who provide clinical services in the traditional dental school setting and those students who provide clinical care in community-based health centers. Nasal MRSA carriage is determined via the presence of the mecA gene isolated from nasal secretions using polymerase chain reaction (PCR). PCR is also used to identify staphylococcal cassette chromosome mec typing (SCCmec) for each identified MRSA strain. SCCmec typing allows for identification of the source of MRSA infection. Hospital-acquired MRSA infection is associated with SCCmec types I, II and III, while community-acquired MRSA is associated with type IV.
One in three (33%) people carry Staphylococcus aureus in their nose, usually without any illness. Two in 100 people (2%) have a colonized case of methicillin-resistant S. aureus (MRSA). Nasal MRSA colonization is a major factor in the development of infectious disease, as it can be routinely transferred to other sites of the body and can enter the body through direct contact with open wounds. There is also risk for transmission via hand carriage, especially with poor hand hygiene. Nasal carriage is not an infectious disease in itself; however, carriers are at risk of self-contamination and transmission to others. Self-inoculation has been established as a mechanism for MRSA transmission and infection. Individuals with MRSA colonization have an estimated three-fold increased risk for developing infection. Persistent MRSA carriage increases risk for contracting MRSA infection for both the healthcare provider and others who are in close proximity. There is increasing evidence that MRSA is present in dental settings, including in dental patients, on dental surfaces, and in dental healthcare workers, including students. The mean rate of nasal MRSA carriage is approximately 4% among health care professionals. To date, there is a lack of well-designed studies documenting nasal MRSA carriage rates among dental professionals. Three recent studies conducted in separate universities found that dental students have nasal MRSA colonization rates at levels that are higher than the general population. In each of these studies, there were marked differences in the percentage of those affected among students in their first and second year as compared to students in their third and fourth year of dental school. Typically, students do not begin to see patients until the end of their second year or at the start of their third year. Clinical exposure to patients is an important risk factor for nasal colonization among dental students. It is unknown whether nasal colonization rates differ between students who provide clinical services in the traditional dental school setting and those students who provide clinical care in community-based health centers. Nasal MRSA carriage is determined via the presence of the mecA gene isolated from nasal secretions using polymerase chain reaction (PCR). PCR is also used to identify staphylococcal cassette chromosome mec typing (SCCmec) for each identified MRSA strain. SCCmec typing allows for identification of the source of MRSA infection. Hospital-acquired MRSA infection is associated with SCCmec types I, II and III, while community-acquired MRSA is associated with type IV.
Conclusion
Nasal MRSA colonization rate was low among this population of dental students. Additional analyses are ongoing on those samples that tested positive for MRSE.
Nasal MRSA colonization rate was low among this population of dental students. Additional analyses are ongoing on those samples that tested positive for MRSE.